The diagnosis of Polycystic Ovary Syndrome (PCOS) is a procedure that has become a controversial issue due to the heterogeneity associated with this pathology, along with the fact that the specific cause is still unclear.
In spite of this, there exists a set of patterns that tend to be commonplace in women with PCOS, and are extremely helpful when it comes to detecting it.
Provided below is an index with the 6 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 4.
- 5.
- 6.
Criteria to diagnose PCOS
In the past, doctors performed a differential diagnosis of PCOS, which means that the first step was to dismiss the presence of other pathologies with similar symptoms to those of PCOS before confirming it. When the results of these tests were negative for other pathologies, the doctor could suspect that the symptoms described by the patient were due to PCOS.
Nonetheless, since year 2003, a new diagnostic protocol was established to confirm whether a woman has PCOS or not: the so-called Rotterdam criteria.
Rotterdam criteria include three of the main symptoms of women with PCOS:
- Oligoovulation or anovulation
- This menstrual alteration involves the presence of cycles that are longer than 35 days, or an absent period for more than 3 months in a row.
- Clinical and/or biochemical hyperandrogenism
- Too elevated androgen levels in blood is called biochemical hyperandrogenism. This can cause clinical signs that are commonplace in women with PCOS, like hirsutism or acne.
- Polycystic ovaries
- Polycystic ovaries characterize for the presence of 12 or more follicles larger than 9 mm, a sign commonly called string of pearls or necklace pattern. An ovarian volume above 10 ml is also an indicator of PCOS.
A woman is diagnosed with PCOS if she has at least 2 of these 3 symptoms.
Diagnostic tests
Normally, women visit a fertility specialist when the menstrual period does not show up, or when they notice certain infertility issues. Given that PCOS is the most common reproductive disorder in women of childbearing age, your doctor will run a series of tests to you to determine whether your symptoms are due to PCOS, including:
Anamnesis & physical exploration
The initial step for diagnosis all diseases is to gather information by asking the patient for her medical history and the symptoms she is experiencing now. This is the definition of anamnesis.
As for PCOS, it is essential for your Obstetrician & Gynecologist to ask the patient for her menstrual periods, as well as other data linked to them. The intake of certain medications in the past few months, as well as the presence of infections or STDs, and the use of birth control methods are also key information.
Also, a physical exploration is required to check if the patient has any clinical sign associated with PCOS. Aspects like the weight, size, and BMI (Body Mass Index) are crucial in this phase.
Excessive body hair growth, especially in areas that are more typical of men, including the face, breasts or back is a disorder called hirsutism, which at the same time is a clinical sign of hyperandrogenism (high androgen levels in blood). For all these reasons, performing a thorough physical examination is crucial before rendering a diagnosis of PCOS.
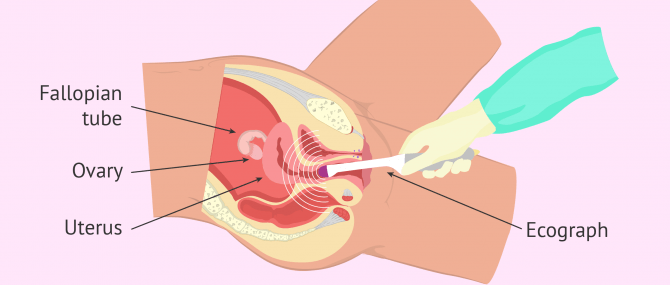
Transvaginal ultrasound
This diagnostic imaging technique is used to check the ovaries, the uterine cavity, and the Fallopian tubes. The ecograph is inserted through the vaginal canal to examine the female reproductive organs more easily.
For this diagnostic test to be successful, the woman should be on her period (basal conditions).
The normal follicle count for women without PCOS ranges between 6 to 12 on each ovary, with a size range of 2-9 mm.
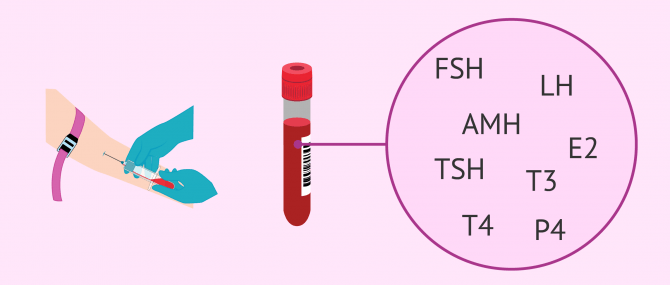
Hormone analysis
Measuring hormone levels is a key step before diagnosing infertility in males and females. Indeed, altered hormone levels cause PCOS.
In the case of PCOS, the main sex hormones are assessed, paying special attention to testosterone and androgens, as well as AMH and LH.
Commonly, the results obtained in women with PCOS are as follows:
- Free testosterone
- When the concentration of free testosterone is equal to or above 50 nanograms per deciliter (ng/dl), it indicates the existence of biochemical hyperandrogenism.
- LH/FSH relationship
- With PCOS, LH levels are abnormally elevated, and can even be 3 times higher than FSH levels.
- AMH levels
- This hormone is produced by antral follicles, which are observed through ultrasound in basal conditions. If AMH levels are higher than 3.5 nanograms per milliliter (ng/ml), it can be due to the presence of multiple follicles in the ovaries. This is a potential indicator of PCOS.
Other hormones such as prolactin, thyroid, or insulin are checked as well.
Again, it is crucial for the woman to be on her period in order for the assessment of these hormones to be properly assessed.
Laparoscopic surgery
This surgical procedure is a surgical procedure used to examine the ovaries using an optical system. A series of incisions are done in the abdomen, allowing the passage of surgical instruments. Laparoscopy is done under general anesthesia.
Polycystic ovaries are characterized for the presence of scar tissue caused by the follicles that do not ovulate. This causes the ovarian cortex to thicken and harden.
With a laparoscopy, examining the aspect of the ovaries to determine if they present signs of PCOS is easier.
This technique is used when none of the above tests have lead to a conclusive diagnosis.
Considering seeing a fertility specialist? Don't forget that, in the field of Reproductive Medicine, as in any other medical area, it is crucial that patients rely on the doctors and staff that will help them through their treatment cycle. Logically, conditions vary from clinic to clinic. For this reason, we recommend that you generate your Fertility Report now. It will offer you a list of clinics that have passed our rigorous selection process successfully. Furthermore, the system will make a comparison between the fees and conditions of each clinic so that you can make a better-informed decision.
FAQs from users
Can PCOS be detected with a genetic analysis?
No, this option is not a viable one presently. Although the results of a number of scientific studies have confirmed the presence of a genetic factor that is highly associated with PCOS, the particular genes causing this endocrine disorder are still unknown.
Can PCOS start at any age?
Obviously, it is necessary that the woman has gone through menarche, that is, the first occurrence of menstruation. Nonetheless, this disorder is typically detected at ages 25 to 30 due to the high number of fertility problems associated and the difficulties it causes in women of childbearing age to get pregnant.
Why does PCOS cause hirsutism?
Hirsutism appears as a consequence of high androgen levels in blood. One of the functions of androgens, such as testosterone, is to grow hair in sites that are more typical of men. If the levels of these hormones are too elevated, it is normal that the woman has more hair than usual.
Suggested for you
Having polycystic ovaries is a typical symptom of PCOS. However, the presence of a single characteristic does not mean that a woman has PCOS by default. Want to learn more about the difference between PCOS and PCO? Click here: What Is the Difference between PCOS & Polycystic Ovaries?
A key test to render a correct diagnosis of PCOS is an analysis of hormone levels, as the ovarian cycle depends on sex hormones and their quantity. To learn more about female fertility tests, read: Female Fertility Tests – How Do You Know if You Can’t Get Pregnant?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Adams Hillard PJ. Oral contraceptives and the management of hyperandrogenism - polycystic ovary syndrome in adolescents. Endocrinol Metab Clin N Am 2005; 34:677-705.
Checa Vizcaíno, M.A., Espinós Gómez, J.J., Matorras Weining, R. (2005). Síndrome del ovario poliquístico. Buenos Aires; Madrid: Médica Panamericana. Sociedad Española de Fertilidad (SEF). ISBN 84-7903-599-4.
ESHRE/ASRM Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril 2004; 81:19-25.
Huddelston HG (2013). Biomarkers of ovarian reserve in women with polycystic ovary syndrome. Semin Reprod Med.
Zawadski JK, Dunaif A. Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. En: Dunaif A, Givens JR, Haseltine FP, Merriam GR (eds.). Polycystic ovary syndrome. Boston: Blackwell Scientific Publications. 1992:377-384.
FAQs from users: 'Can PCOS be detected with a genetic analysis?', 'Can PCOS start at any age?' and 'Why does PCOS cause hirsutism?'.
Author